Availity Clearinghouse Rejection Codes
Availity Clearinghouse Rejection Codes - To determine whether any of the payers that you submit to require a contract, see the availity payer list. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is.
Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list.
Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list.
Check Rejections in Availity
To determine whether any of the payers that you submit to require a contract, see the availity payer list. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is.
Clearinghouse Rejection Codes [EXPLAINED] BellMedEx
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. To determine whether any of the payers that you submit to require a contract, see the availity payer list.
Meet Availity Our New & Improved Clearinghouse 30 less than current
Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list.
8 Common Clearinghouse Rejection Codes Debunked — Etactics
Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list.
Clearinghouse Rejection Codes [EXPLAINED] BellMedEx
Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. To determine whether any of the payers that you submit to require a contract, see the availity payer list. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is.
Clearinghouse Rejection Codes & How To Fix Them? BMB
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. To determine whether any of the payers that you submit to require a contract, see the availity payer list.
Clearinghouse Rejection Codes Explained [Latest 2025]
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. To determine whether any of the payers that you submit to require a contract, see the availity payer list.
Clearinghouse Rejection Codes [EXPLAINED] BellMedEx
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. To determine whether any of the payers that you submit to require a contract, see the availity payer list.
8 Common Clearinghouse Rejection Codes Debunked — Etactics
To determine whether any of the payers that you submit to require a contract, see the availity payer list. Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is.
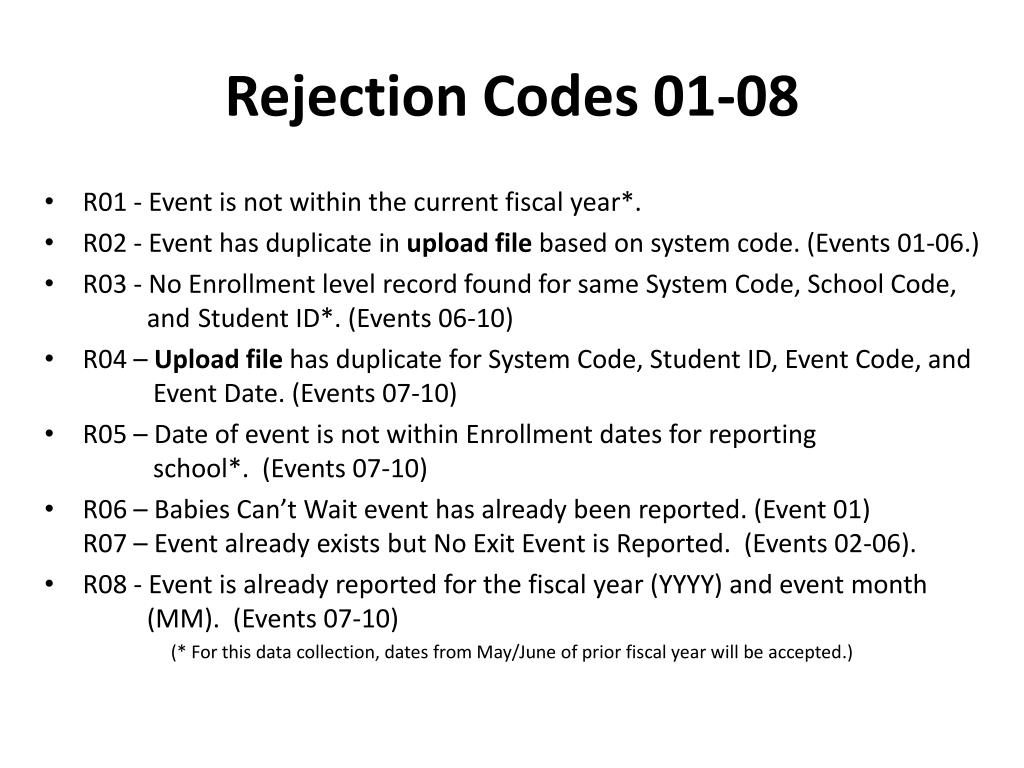
PPT Cultivating the Special Education Event Garden PowerPoint
Availity simplifies payer connectivity and claim submission with expert support for edi transactions, payer ids, and healthcare. Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list.
Availity Simplifies Payer Connectivity And Claim Submission With Expert Support For Edi Transactions, Payer Ids, And Healthcare.
Claims may reject when the secondary insurance does not contain a valid payer id, or if the claim filing indicator is. To determine whether any of the payers that you submit to require a contract, see the availity payer list.

![Clearinghouse Rejection Codes [EXPLAINED] BellMedEx](https://bellmedex.com/wp-content/uploads/2024/10/blog-Fi.jpg)

![Clearinghouse Rejection Codes [EXPLAINED] BellMedEx](https://bellmedex.com/wp-content/uploads/2024/10/blog-info-1-905x1024.jpg)

![Clearinghouse Rejection Codes Explained [Latest 2025]](https://rcmfinder.com/wp-content/uploads/2025/01/Clearinghouse-Rejection-Codes-Explained.jpg)
![Clearinghouse Rejection Codes [EXPLAINED] BellMedEx](https://bellmedex.com/wp-content/uploads/2024/02/what-is-an-entity-code-rejection.jpg)