Pcp Services Not Available Meaning
Pcp Services Not Available Meaning - This denial occurs when the provider who rendered the service is not contracted with the insurance. You can get many services without a referral from your primary care provider (pcp). Denial code 243 means services were not approved by your network or primary care providers. If you disagree with that denial, you. Learn how to resolve this issue and. This means that your pcp does not need to arrange or approve. In an hmo, every thing goes through your designated pcp. In this scenario, the claim can be. While some revisions may be inevitable, for example if a person has an. Yes, the payer is indicating that the services did need some kind of authorization or referral.
If you disagree with that denial, you. Denial code 243 means services were not approved by your network or primary care providers. In an hmo, every thing goes through your designated pcp. Learn how to resolve this issue and. If the pcp wasn't accepting new patients, you had to register a new pcp with. In this scenario, the claim can be. Yes, the payer is indicating that the services did need some kind of authorization or referral. This denial occurs when the provider who rendered the service is not contracted with the insurance. You can get many services without a referral from your primary care provider (pcp). This means that your pcp does not need to arrange or approve.
Denial code 243 means services were not approved by your network or primary care providers. In this scenario, the claim can be. This means that your pcp does not need to arrange or approve. You can get many services without a referral from your primary care provider (pcp). In an hmo, every thing goes through your designated pcp. While some revisions may be inevitable, for example if a person has an. Learn how to resolve this issue and. Yes, the payer is indicating that the services did need some kind of authorization or referral. If you disagree with that denial, you. This denial occurs when the provider who rendered the service is not contracted with the insurance.
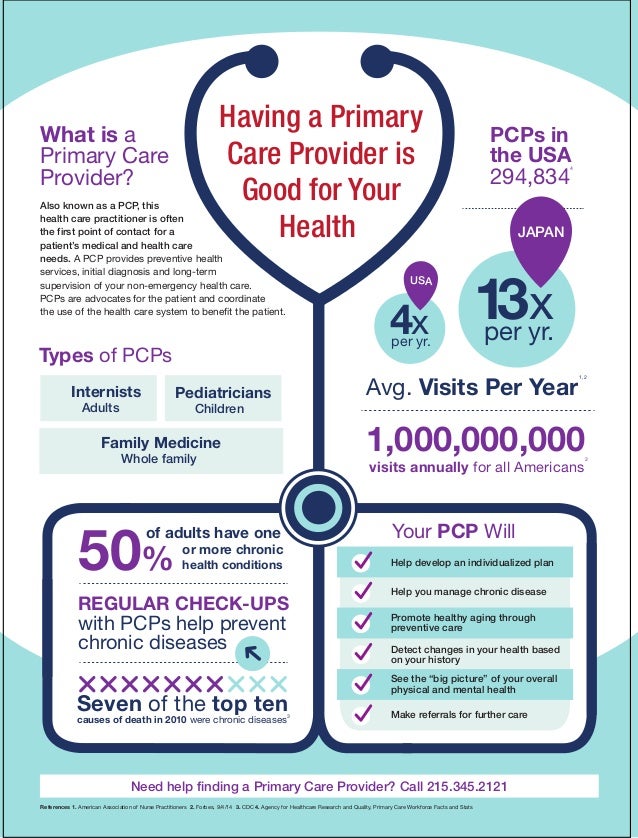
Primary careproviderinfographic
Learn how to resolve this issue and. You can get many services without a referral from your primary care provider (pcp). In an hmo, every thing goes through your designated pcp. In this scenario, the claim can be. If the pcp wasn't accepting new patients, you had to register a new pcp with.
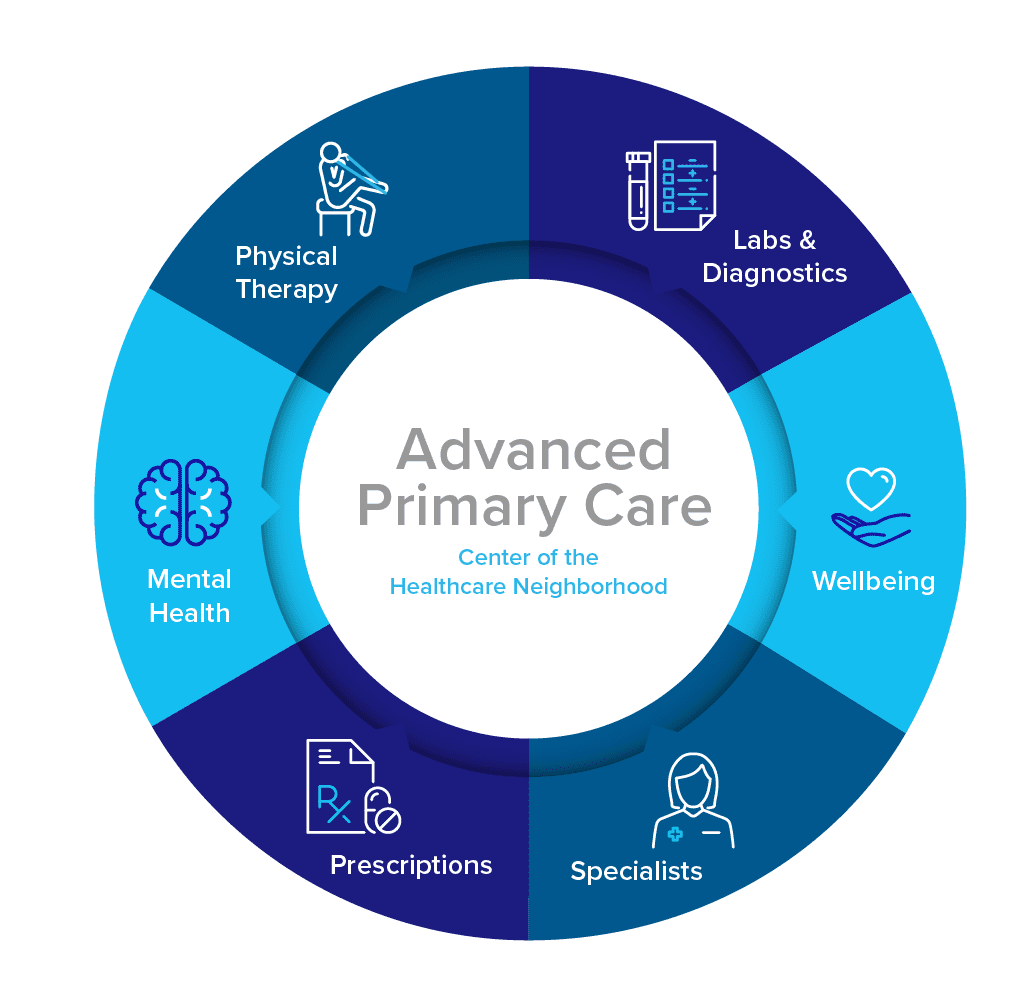
Four myths you've heard about Advanced Primary Care Proactive MD®
In an hmo, every thing goes through your designated pcp. If you disagree with that denial, you. Learn how to resolve this issue and. Yes, the payer is indicating that the services did need some kind of authorization or referral. This means that your pcp does not need to arrange or approve.
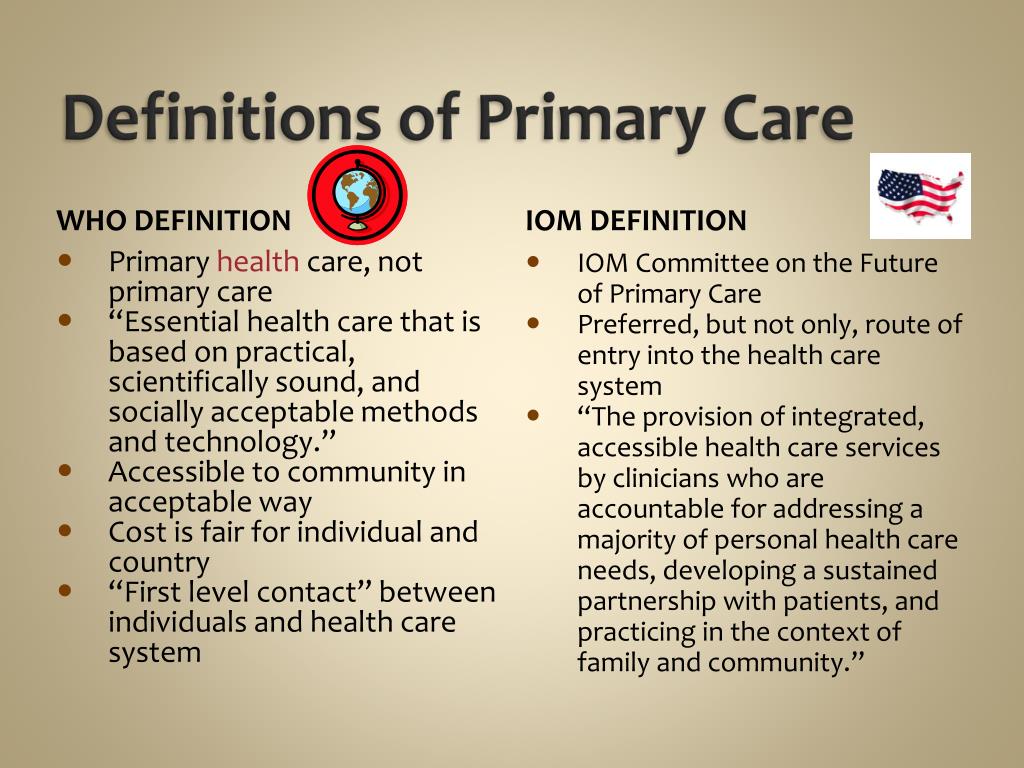
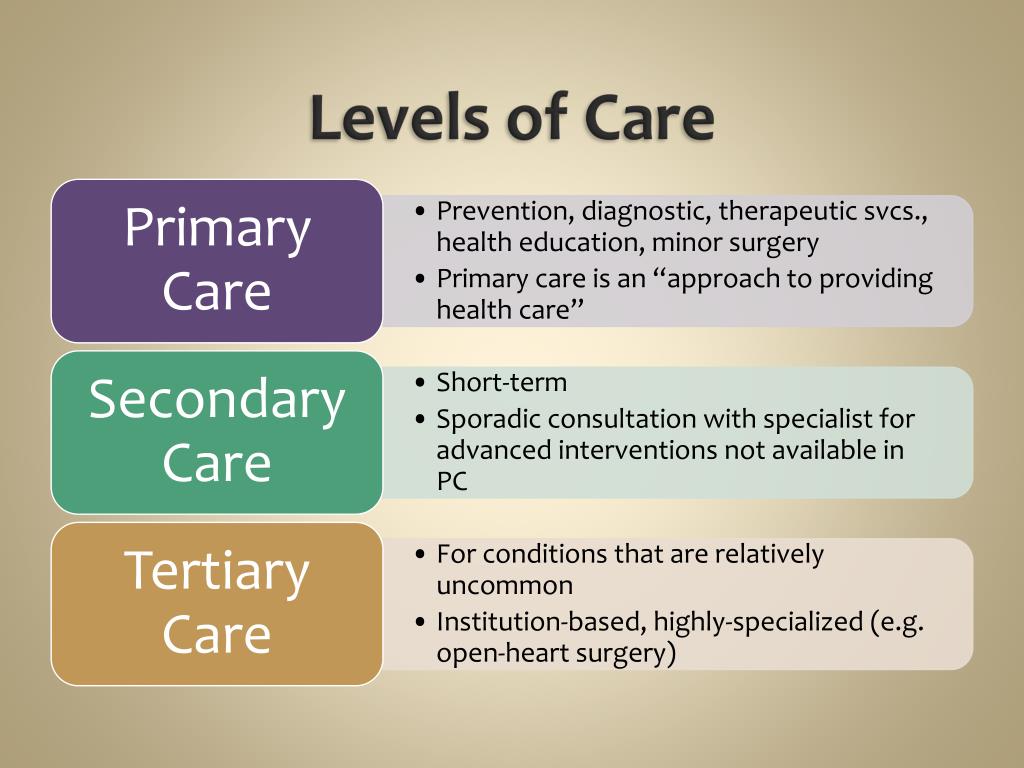
PPT Chapter 7 Outpatient Services and Primary Care PowerPoint
Learn how to resolve this issue and. This means that your pcp does not need to arrange or approve. In an hmo, every thing goes through your designated pcp. Denial code 243 means services were not approved by your network or primary care providers. If you disagree with that denial, you.
Primary Care Providers Horizon Health
You can get many services without a referral from your primary care provider (pcp). While some revisions may be inevitable, for example if a person has an. In this scenario, the claim can be. This means that your pcp does not need to arrange or approve. If the pcp wasn't accepting new patients, you had to register a new pcp.
Explained What Is 503 Service Not Available? A Quick Guide Cashify Blog
In this scenario, the claim can be. This denial occurs when the provider who rendered the service is not contracted with the insurance. You can get many services without a referral from your primary care provider (pcp). Denial code 243 means services were not approved by your network or primary care providers. Yes, the payer is indicating that the services.
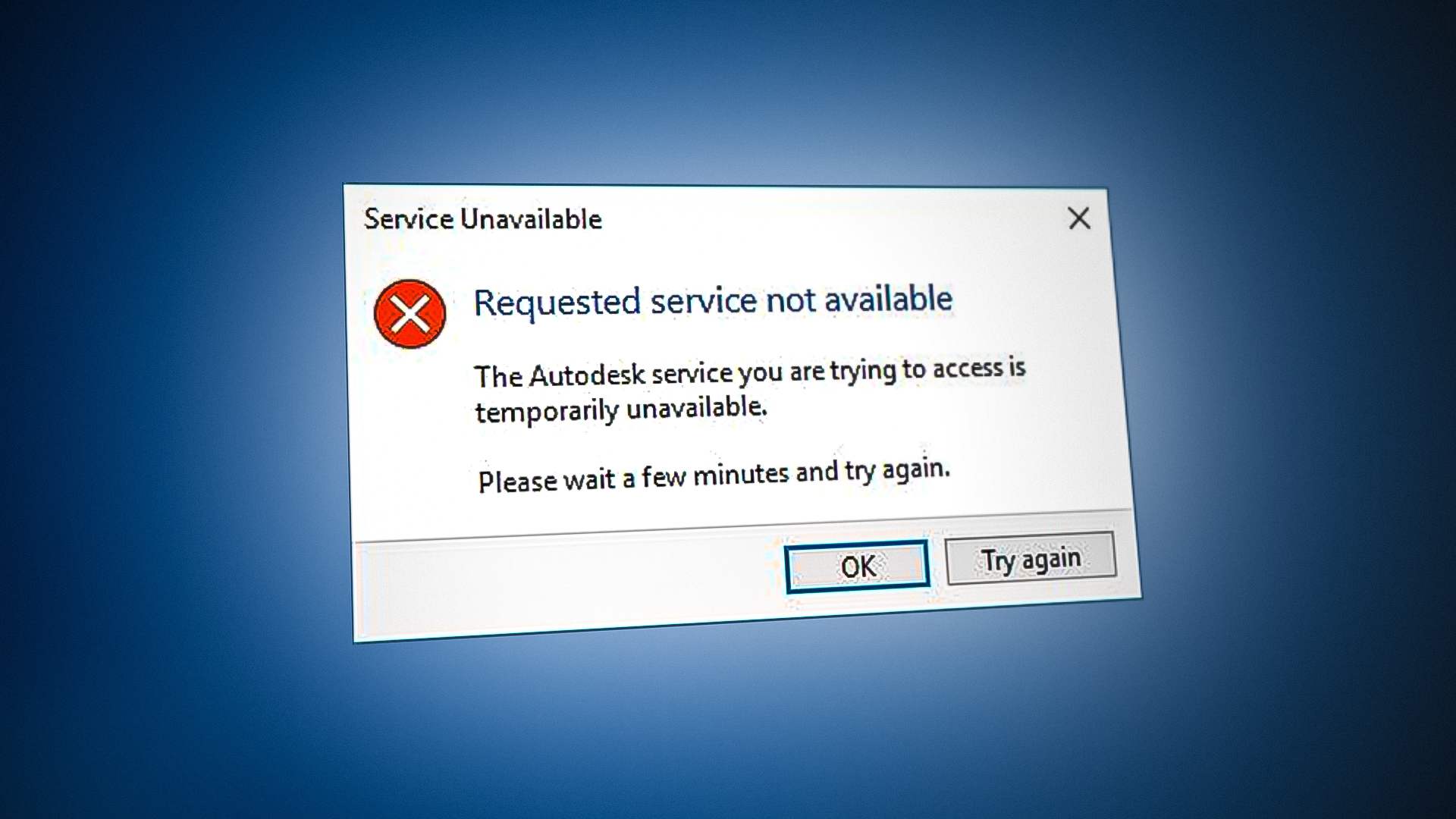
How to Fix Autodesk Issue Requested Service Not Available
Learn how to resolve this issue and. If the pcp wasn't accepting new patients, you had to register a new pcp with. While some revisions may be inevitable, for example if a person has an. This means that your pcp does not need to arrange or approve. In this scenario, the claim can be.
NHS England » Social prescribing Reference guide and technical annex
In this scenario, the claim can be. In an hmo, every thing goes through your designated pcp. Learn how to resolve this issue and. This denial occurs when the provider who rendered the service is not contracted with the insurance. You can get many services without a referral from your primary care provider (pcp).
PPT Chapter 7 Outpatient Services and Primary Care PowerPoint
In this scenario, the claim can be. In an hmo, every thing goes through your designated pcp. Learn how to resolve this issue and. Denial code 243 means services were not approved by your network or primary care providers. If you disagree with that denial, you.
Third Party Payers Direct Payment is when the patient pays for pharmacy
This denial occurs when the provider who rendered the service is not contracted with the insurance. You can get many services without a referral from your primary care provider (pcp). While some revisions may be inevitable, for example if a person has an. In an hmo, every thing goes through your designated pcp. Denial code 243 means services were not.
Detroit VA Medical Center Department of Medicine Pearls for Patient
In an hmo, every thing goes through your designated pcp. Denial code 243 means services were not approved by your network or primary care providers. While some revisions may be inevitable, for example if a person has an. Yes, the payer is indicating that the services did need some kind of authorization or referral. You can get many services without.
While Some Revisions May Be Inevitable, For Example If A Person Has An.
Learn how to resolve this issue and. In an hmo, every thing goes through your designated pcp. Denial code 243 means services were not approved by your network or primary care providers. This denial occurs when the provider who rendered the service is not contracted with the insurance.
This Means That Your Pcp Does Not Need To Arrange Or Approve.
If the pcp wasn't accepting new patients, you had to register a new pcp with. Yes, the payer is indicating that the services did need some kind of authorization or referral. You can get many services without a referral from your primary care provider (pcp). In this scenario, the claim can be.


.jpg)
